Living with type 2 diabetes can feel overwhelming, especially when trying to maintain stable blood sugar levels each day. But the good news? A structured, healthy daily routine can make a significant difference in controlling blood glucose naturally—without constant medication adjustments.
As a licensed pharmacist, I’ve worked closely with countless patients managing type 2 diabetes. What I’ve seen consistently is that simple lifestyle changes, when done consistently, can prevent complications, reduce medication dependence, and improve overall well-being.
In this comprehensive guide, you’ll learn the best daily routine for someone with type 2 diabetes—including actionable steps on diet, exercise, sleep, stress, hydration, and medication management—all grounded in expert medical guidance and real-world clinical insights.
Why Daily Routine Matters in Type 2 Diabetes
Maintaining a structured daily routine helps regulate:
• Blood glucose levels
• Insulin sensitivity
• Energy levels
• Mood and mental focus
Irregular habits—like skipping meals, poor sleep, or inconsistent medication timing—can cause dangerous fluctuations in blood sugar. Building a predictable, well-balanced routine allows your body to stabilize and function optimally.
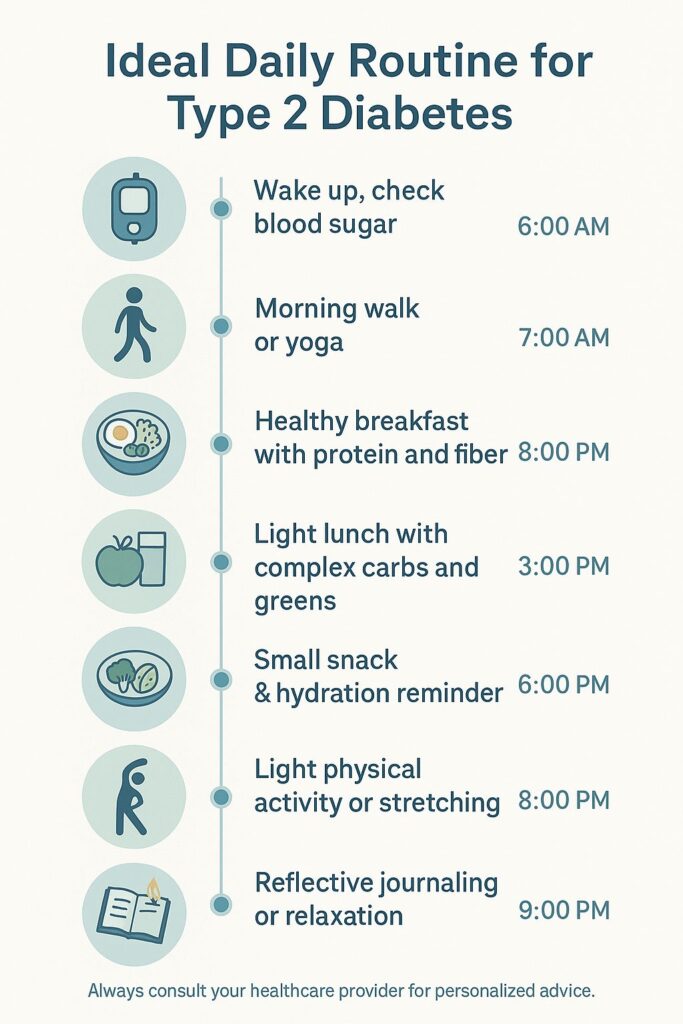
Morning Routine: Start the Day Strong
Wake-Up Time (6:00–7:00 AM)
Consistency is key. Waking up at the same time every day supports circadian rhythm, which is linked to insulin sensitivity.
Tip: Use a smart alarm and avoid hitting snooze—it delays metabolism activation.
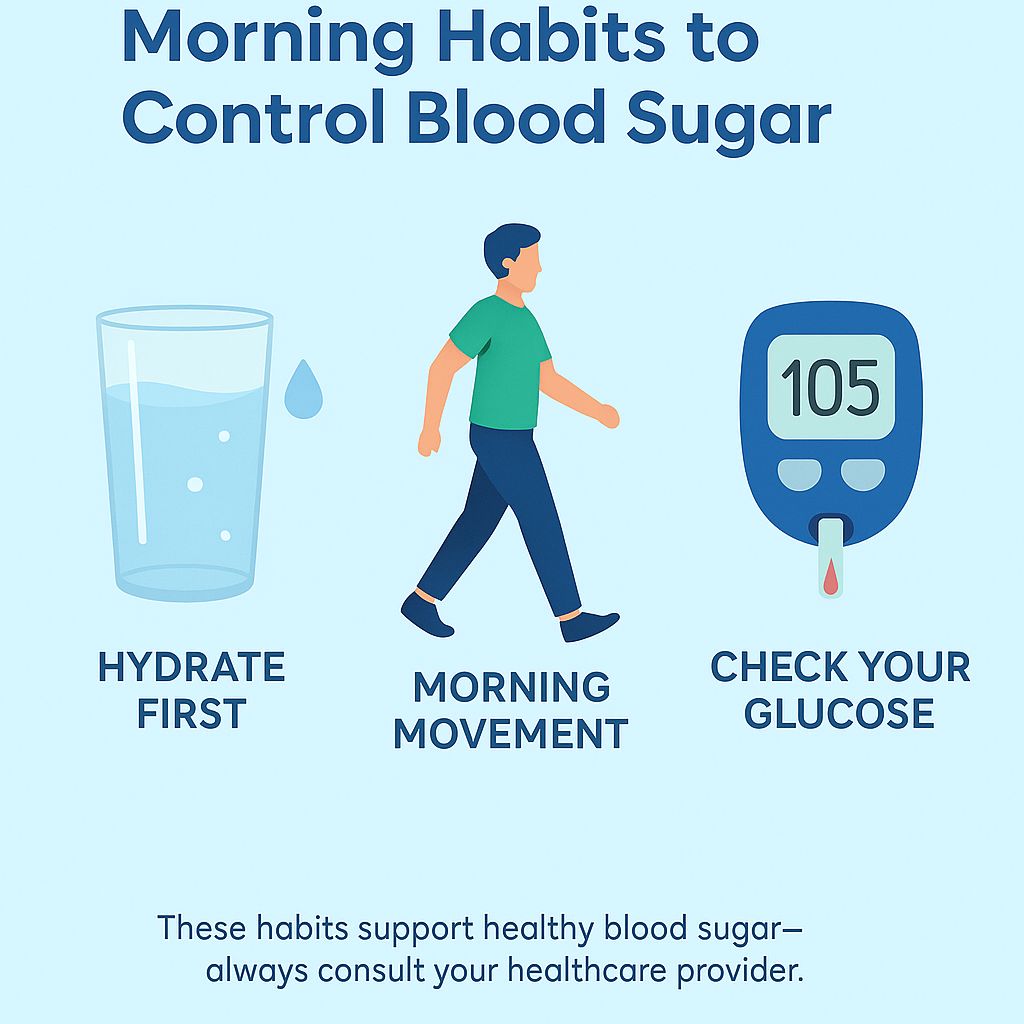
Hydrate First Thing (6:15 AM)
Drink 1–2 glasses of warm water with lemon or fenugreek seeds soaked overnight. Hydration aids digestion, flushes out toxins, and may help reduce morning blood glucose spikes.
Light Exercise or Walk (6:30–7:00 AM)
Engage in light movement such as:
• Brisk walking
• Yoga
• Stretching or tai chi
Benefits:
• Improves insulin sensitivity
• Lowers fasting blood sugar
• Boosts mood and metabolism
Data Point: A study in Diabetes Care showed that morning walks reduce postprandial glucose by 20–25%.
📊 Blood Sugar Check (Before Breakfast)
Use a glucometer to log fasting blood sugar. This helps track patterns and adjust your routine as needed.
Target: 80–130 mg/dL (ADA Guidelines)
Breakfast: The Most Important Meal
Time: Within 1 Hour of Waking
Skipping breakfast increases insulin resistance.
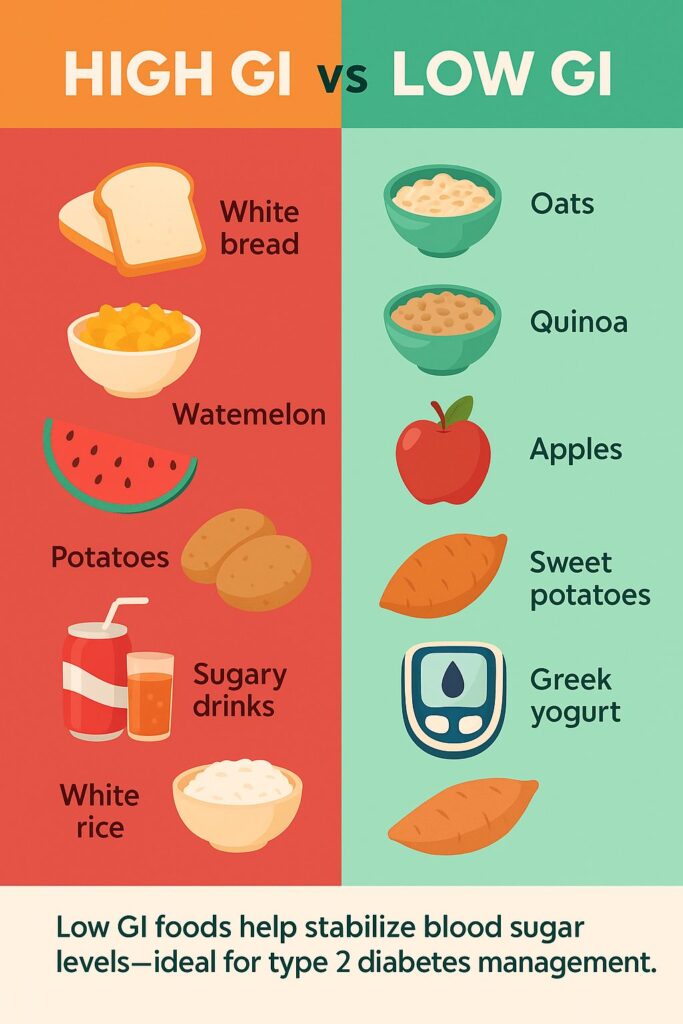
Ideal Diabetic Breakfast Options
• 2 boiled eggs + 1 slice whole-grain toast + avocado
• Steel-cut oats + chia seeds + cinnamon
• Greek yogurt + berries + flaxseeds
• Moong dal chilla with coriander chutney
Nutritional Focus:
• Low glycemic index (GI)
• High in fiber and protein
• Healthy fats
Avoid:
• Sugary cereals
• White bread or pastries
• Fruit juices
External Source: American Diabetes Association – Nutrition Guidelines
Mid-Morning Routine (9:30–10:30 AM)
Movement Break
After sitting for 1–2 hours, do:
• 5-minute walk
• Seated leg raises
• Arm stretches
Why? Prolonged sitting spikes blood sugar.
Diabetic-Friendly Snack (Optional)
If hungry:
• Handful of unsalted nuts
• Buttermilk or green tea
• Apple with peanut butter
Midday Routine (12:00–2:00 PM)
Balanced Lunch Ideas
• Grilled chicken/fish + brown rice + sautéed veggies
• Mixed lentils (dal) + millet roti + cucumber salad
• Quinoa bowl + paneer + greens
Macronutrient Ratio:
• 40% low-GI carbs
• 30% lean protein
• 30% healthy fats
Table: Sample Macronutrient Distribution for Diabetics
| Food Group | Ideal % | Example Sources |
| Carbs Low GI | 40% | Quinoa, brown rice, sweet potatoes |
| Proteins | 30% | Eggs, legumes, fish, paneer |
| Fats | 30% | Avocado, olive oil, nuts |
Afternoon Routine (2:30–5:00 PM)
Stress Reduction
Chronic stress elevates cortisol, worsening blood sugar control.
Practices to Try:
• Deep breathing
• Guided meditation (10 mins)
• Gratitude journaling
• Listening to calming music
Optional Glucose Check (Post-lunch)
Especially useful if you’re newly diagnosed or trying a new diet plan.
Evening Routine (5:30–7:30 PM)
Physical Activity (30–45 minutes)
The evening is a great time for moderate-intensity exercise:
• Walking after dinner
• Resistance training
• Dancing or swimming
Study: According to Mayo Clinic, exercise 30 minutes/day, 5 days/week can lower A1C by 0.5% to 1%.
Light Dinner Options

• Stir-fried vegetables + tofu + millet roti
• Grilled fish + cucumber salad + lentil soup
• Moong dal khichdi + spinach + curd
Avoid:
• Overeating
• Heavy carbs like white rice or fried food
• Late-night meals (after 8 PM)
Night Routine: Preparing for Restful Sleep
Wind-Down Ritual (8:30–9:30 PM)
• No screens 1 hour before bed
• Herbal teas (like chamomile or cinnamon)
• Foot massage or warm bath
Final Blood Sugar Check (If Advised)
Speak to your doctor/pharmacist if nighttime hypoglycemia is a concern.
Sleep Time: 10:00 PM (Aim: 7–8 hours)
Poor sleep increases insulin resistance and hunger hormones.
Hack: Use a sleep tracking app to monitor patterns.
Medications and Supplement Reminders
Medication Consistency
• Set fixed times for oral medications (like Metformin, Glipizide)
• Use pill organizers or mobile reminders
Common Supplements
Check with your healthcare provider before using:
• Berberine (may lower blood sugar)
• Cinnamon extract
• Vitamin D3
• Magnesium
External Source: Healthline – Diabetes Supplements
Hydration Throughout the Day
Target: 2.5–3 liters daily
• Start morning with water
• Add cucumber or lemon for flavor
• Avoid sugary drinks, limit caffeine
Things to Avoid in a Diabetic Routine
Daily Routine Mistakes
1. Skipping meals
2. Late dinners
3. Stress binge eating
4. Sedentary lifestyle
5. Unmonitored blood sugar
Key Takeaways
• Routine is the foundation of diabetes management.
• Eat low-GI, balanced meals at regular intervals.
• Prioritize morning movement and evening exercise.
• Monitor blood sugar consistently, especially before/after meals.
• Manage stress, stay hydrated, and get quality sleep.
A pharmacist-guided, structured routine empowers you to stay ahead of complications and live a fuller, healthier life.
Frequently Asked Questions (FAQs)
Can I skip breakfast if I’m not hungry?
No. Skipping breakfast can increase insulin resistance. Opt for a small, protein-rich meal even if not very hungry.
How often should I check my blood sugar?
Check fasting and post-meal sugar initially. Frequency depends on your doctor’s advice and medication type.
Is walking alone enough as exercise?
Yes, especially if done for 30–45 mins daily. Add resistance training twice a week for optimal benefits.
Can I drink tea or coffee?
Yes, in moderation. Avoid sugar and use low-fat milk or plant-based options. Herbal teas are even better.
What if I have night-time cravings?
Opt for a small protein snack like a boiled egg or nuts. Avoid carbs and sugary snacks before bed.
Medical Disclaimer
This article is for educational purposes only and does not substitute for professional medical advice. Always consult your doctor, pharmacist, or certified diabetes educator before making any changes to your treatment or lifestyle.


Pingback: Understanding the Causes of Diabetes: A Pharmacist’s Expert Perspective - Pharma Heals
Pingback: Diabetes Test Kit Guide for Accurate Home Monitoring - Pharma Heals
Pingback: Diabetes Yoga Exercises: Evidence-Based Poses to Improve Blood Sugar Control and Overall Health - Pharma Heals
Pingback: Overnight Oats for Diabetes: How This Simple Breakfast Can Help Stabilize Your Blood Sugar Levels - Pharma Heals
Pingback: Diabetes Test at Home Guide for Accurate Results - Pharma Heals
Pingback: Is Papaya Good for Diabetes: Evidence-Based Benefits and Blood Sugar Impact - Pharma Heals