As a licensed pharmacist, I’ve worked with countless individuals managing diabetes or prediabetes. One pattern that consistently stands out is how transformative morning routines can be. Whether you’re newly diagnosed or have been managing diabetes for years, understanding and optimizing your morning habits to control blood sugar can set the tone for a healthier day.
Your body’s hormonal landscape shifts in the early hours, triggering natural glucose elevations, often called the “dawn phenomenon.” How you respond during this time — through food, activity, stress management, and medication timing — can significantly impact your fasting glucose levels, insulin sensitivity, and energy throughout the day.
In this comprehensive guide, I’ll share medically grounded, pharmacist-approved strategies for building the best morning routine for blood sugar — one that blends science with practicality, supports emotional well-being, and helps you regain control over your health.
Understanding Morning Blood Sugar Spikes
Many people wake up surprised to find that their fasting blood sugar is higher than expected, despite avoiding food overnight. This often stems from natural hormonal fluctuations, sleep disturbances, or poorly matched evening medications.
Factors that raise morning blood glucose:
• Dawn phenomenon (discussed below)
• Somogyi effect (rebound hyperglycemia from overnight lows)
• High-carb or late-night meals
• Sedentary lifestyle
• Poor sleep quality or sleep apnea
• Medication timing mismatches
Regularly elevated morning blood sugar can:
• Worsen insulin resistance
• Lead to fatigue and brain fog
• Increase HbA1c over time
• Raise cardiovascular risk
The Science of the Dawn Phenomenon
What Is It?
The dawn phenomenon refers to a surge in blood sugar levels that occurs naturally between 4 AM and 8 AM, even in people without diabetes.
Why Does It Happen?
• Hormones released early in the morning — including cortisol, glucagon, growth hormone, and adrenaline — stimulate the liver to release stored glucose.
• This results in a rise in fasting blood sugar, especially problematic for those with insulin resistance or impaired pancreatic function.
Supporting Data:
A study published in the Journal of Clinical Endocrinology & Metabolism found that up to 50% of people with type 2 diabetes experience elevated morning blood glucose due to the dawn phenomenon.
12 Proven Morning Habits to Control Blood Sugar

Let’s explore the most effective and pharmacist-approved morning rituals for diabetes control, broken into categories for clarity and action.
1. Wake Up at a Consistent Time (7 Days a Week)
• Irregular sleep disrupts circadian rhythm and insulin sensitivity.
• Studies show consistent wake/sleep cycles help regulate cortisol and glucose.
Tip: Set a wake-up alarm within a 30-minute window, even on weekends.
2. Start Your Day With Movement
Light physical activity boosts muscle glucose uptake and insulin sensitivity. This can dramatically lower morning blood sugar.
Options:
• 20–30 min brisk walk
• 10–15 min yoga or tai chi
• Home circuit: squats, pushups, walking lunges
Data Point: According to Diabetes Care, 20 minutes of morning walking can lower post-breakfast glucose by 20–25%.
3. Eat a Low-Glycemic, High-Protein Breakfast
Skipping breakfast can lead to insulin resistance and mid-morning spikes. Choose foods with fiber, protein, and healthy fats.
Best Options:
• Steel-cut oats with walnuts and chia
• Greek yogurt with flaxseeds and berries
• Boiled eggs with multigrain toast
• Indian options: moong dal chilla, vegetable upma, besan cheela
Avoid:
• Fruit juices
• Refined cereals
• White bread
• Sugary coffee drinks
4. Hydrate Before Anything Else
Your body is mildly dehydrated in the morning. Water helps flush excess glucose through the kidneys and supports cellular insulin function.
Pharmacist Tip: Drink 1–2 glasses of warm water, optionally infused with:
• Lemon juice
• Cinnamon
• Fenugreek seeds (soaked overnight)
5. Check Your Fasting Blood Sugar
Monitoring helps you track trends and adjust your morning strategy.
• Fasting range (ADA): 80–130 mg/dL
• Use a glucometer or continuous glucose monitor (CGM)
• Log results to share with your healthcare provider
6. Practice Mindful Stress Reduction
High cortisol = high glucose. Mindfulness can reduce stress and lower blood sugar.
Effective Morning Techniques:
• Deep breathing (5–10 minutes)
• Morning meditation (Headspace, Calm apps)
• Journaling or gratitude writing
• Gentle stretching or nature walks
Mayo Clinic research shows that regular meditation can reduce fasting blood sugar by up to 10 mg/dL.
7. Choose Your Morning Beverage Wisely
Caffeine can be a double-edged sword. Monitor your reaction carefully.
Approved Options:
• Green tea
• Black coffee (without sugar or creamers)
• Cinnamon water
• Herbal teas: tulsi, ginger, fenugreek
Avoid:
• Sugary chai
• Flavored lattes
• Packaged smoothies
8. Avoid Immediate Screen Exposure
Blue light and early exposure to stressful content (emails, news, social media) spike cortisol.
Solution:
• Delay screen time by 30–60 minutes
• Use this time for calm, focused activities
9. Time Your Medications Properly
As a pharmacist, I stress the importance of medication timing:
• Take metformin or insulin as prescribed
• Some meds work best before breakfast
• Use reminders or apps (e.g., Medisafe)
Consult your doctor if you’re unsure about food/medication interaction.
10. Plan Your Day (Mentally or on Paper)
Mental clarity reduces stress and improves decision-making around food, activity, and self-care.
• Write down top 3 priorities
• Include planned meals and glucose checks
• Visualize success
11. Consider Natural Supplements (With Caution)
Some natural aids can support glucose metabolism.
Evidence-backed options:
• Cinnamon extract (500–1000 mg)
• Berberine
• Fenugreek seed
• Alpha-lipoic acid
Warning: Always consult a doctor or pharmacist before combining with prescription meds.
12. Review Your Sleep Quality
What happened last night directly affects your blood sugar today.
Track sleep with apps like:
• Fitbit
• Apple Health
• Sleep Cycle
Aim for 7–9 hours with consistent bedtime routines.
Morning Routines to Avoid
| Habit | Why to Avoid |
| Skipping breakfast | Causes insulin resistance, cravings |
| Sugary coffee | Spikes glucose and cortisol |
| Immediate phone use | Raises stress |
| Skipping hydration | Increase glucose concentration |
| Being sedentary | Reduce insulin effectiveness |
Low-Glycemic Breakfast Examples
| Food | Glycemic Index | Notes |
| Steel-cut oats | 55 | Add cinnamon or nuts |
| Boiled eggs | 0 | Pair with whole grains |
| Chia pudding | <45 | Rich in fiber & omega-3 |
| Moong dal chilla | ~40 | High protein indian option |
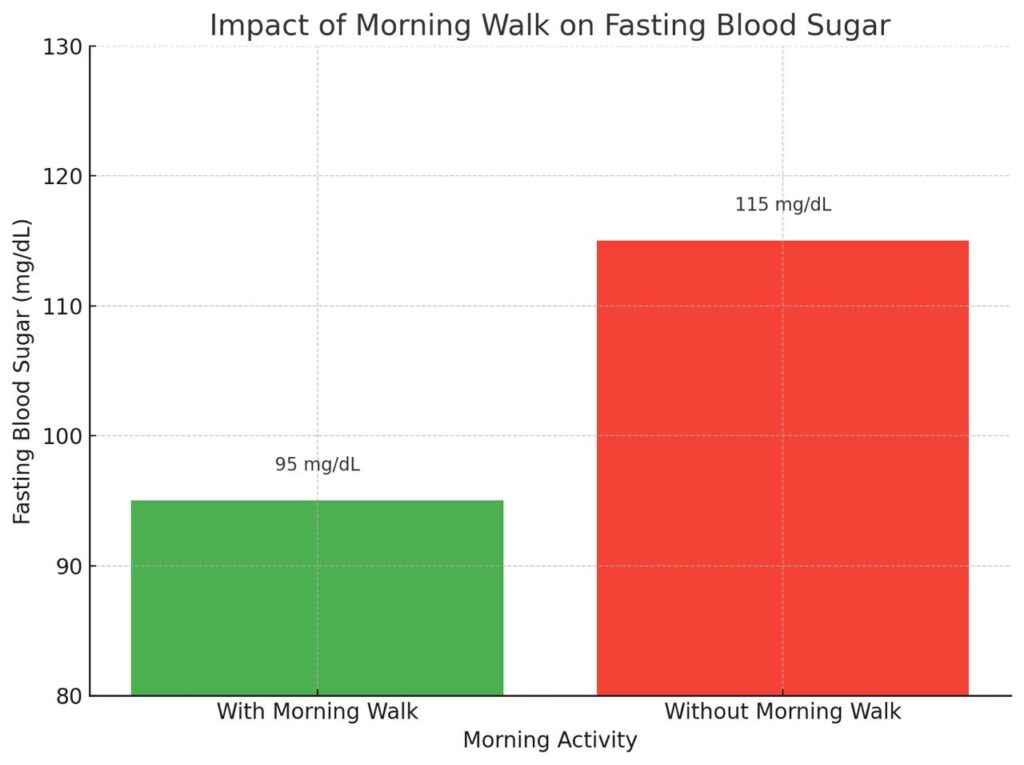
“Impact of Morning Walk on Fasting Blood Sugar.” It compares:
• With Morning Walk: 95 mg/dL (green)
• Without Morning Walk: 115 mg/dL (red)
Expert Tips: Medications, Monitoring & Adjustments
• Time your blood sugar checks at consistent times daily.
• Keep a glucose log — apps like MySugr or Diabetes:M are pharmacist-approved.
• Always discuss changes in routine or supplements with your endocrinologist or diabetes educator.
Frequently Asked Questions (FAQs)
Why is my blood sugar high in the morning if I haven’t eaten?
This is likely due to the dawn phenomenon, where early morning hormones raise glucose levels.
Can walking after waking up really lower my blood sugar?
Yes. Even 15–20 minutes of walking can improve muscle glucose uptake, lowering your fasting levels.
What is the best breakfast for morning blood sugar control?
Choose meals that are low-GI, high-protein, and high in fiber, like oatmeal with chia or moong dal chilla.
Should I skip breakfast to lower blood sugar?
No. Skipping breakfast often leads to higher insulin resistance and post-meal glucose spikes.
Does coffee increase morning blood sugar?
It can in some people. Monitor your response and avoid added sugars or creamers.
Key Takeaways
• Your morning habits directly shape your daily blood sugar control.
• Focus on routine, movement, hydration, and nutrition.
• Monitor trends and talk to your provider before making changes.
• Small, consistent changes lead to lasting results.
References & External Resources
• American Diabetes Association – Managing Blood Sugar
• Mayo Clinic – Diabetes Management
• Healthline – Diabetes and the Dawn Phenomenon
Medical Disclaimer
This article is intended for educational purposes only. It is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your doctor, pharmacist, or certified diabetes educator before making changes to your diabetes care plan.




Pingback: Frequent Urination Diabetes: Causes, Symptoms, and Effective Management - Pharma Heals
Pingback: Control Blood Sugar Levels at Home with Natural Remedies: Complete Guide - Pharma Heals
Pingback: Overnight Oats for Diabetes: How This Simple Breakfast Can Help Stabilize Your Blood Sugar Levels - Pharma Heals
Pingback: Diabetes Test at Home Guide for Accurate Results - Pharma Heals
Pingback: Why Is Fasting Sugar Normal But Post-Meal Sugar High? Causes Explained - Pharma Heals